74 YM WITH LOSS OF SPEECH , URINARY INCONTINENCE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
Blog by Janhavi Virani ( GM intern )
A 74 year old male who is resident of kondaram ( Dist- Nalgonda) , an agricultural labourer ( cotton , paddy ) was referred from outside hospital i/v/o
1. loss of speech since 10 days
2. Urinary incontinence since 10 days
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 25 years back
1.25 years back he went to Bombay at her sisters home while returning back to kondaram got fever for a 1 week which relieved with medication and on routine investigations was found to have Diabetes Mellitus for which he was started on ORAL HYPOGLYCAEMC DRUGS
2. Patient was asymptomatic 17 years then he developed pedal Edema till knees, yellowish discolouration of eyes and shortness of breadth on exertion for which he got admitted to hospital for 8 days and was managed conservatively.
3. Patient was asymptomatic for 7 years back then 10 years back he developed, history of fever which was low grade associated with evening rise of temperature and cough for 10 days
Diagnosed with ? Sputum positive Tuberculosis and was treated with ATT for 2 years
4. He was asymptomatic till 3years back he then developed pain in the right loin for 10 days for which they went to a local hospital and were told as having renal calculi and was kept on conservative management but pain did not subside pain didn’t subsided even on using medication for 6 days and then ?stent /?foleys was placed ,but still his pain didn’t subsided associated with new onset fever,and then they removed the placed stent ,but still the pain at the right loin persisted a surgery was done?lithotripsy ,and then again went to other hospital as they were told that calculi wasn’t removed completely and again stent was placed >>it got infected and seen as pus filled mass at the right loin and then surgery was done and pain got relieved
5. Patient was alright till 4 months then he had small abrasion / small crack over left toe initially And then he got injury over the same finger by accidentally hitting it to a wall lead to —> swelling —>backish discolouration in 8 days —> amputation of 2nd toe
At the same time patient developed dragging type of pain in the left hand for which investigations were done and treated with muscle relaxants and PPI .
After 2 days had history of fall ( due to imbalance) at 2:00am in night when he got up to go to washroom for which went to hospital and was found to have ? intertrochantric fracture ? Hemiarthroplasty was done
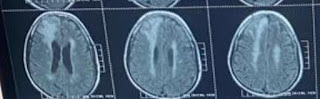
During postoperative period patient had episodes of altered sensorium over a transient period , for which MRI/CT was done was told to have mass in the brain (? Neoplasm)
and the episodes of altered sensorium/hallucinations once/twice in a week(Eg:He mistakened the hanged clothes as persons,and used to talk with persons who expired)
And 2 months ago ,he developed pain in the right hypochondrium dragging type and got admitted in hospital and was treated conservatively for 10 days,and told as having ?cholelithiasis ,and
10 days ago in the afternoon he ate rice and at 3:00pm he had a pomegranate fruit and at 4:00pm he was sleeping on the bed and when his wife called her,he had no response on calling him(lost his speech),(eyes open )and she thought it as hypoglycaemic episode and poured sugar in his mouth but he was not having it,and at the same time he had involuntary rolling over the bed and stiffened mouth(unable to open) and had involuntary micturition at that time and rmp arrived and his Bp and grbs was normal and they took them to hospital and during travelling he had deviation of mouth to right, they(attenders)thought it as hemiparesis, and at hospital his SBP was 240mmHg, and on medication the deviation got corrected and on day 2 of admission due to decrease in saturation ,patient was intubated on 8-7-2023 and extubated on 14-07-2023.
Post extubation,no return of his speech and there were absent tongue moments also.
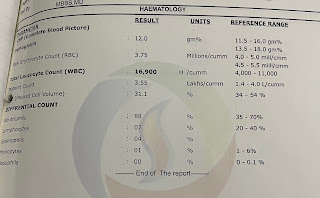
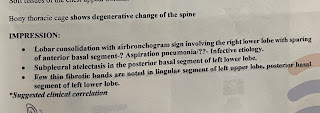
Investigations- (09/07/2023)
On 10/07/2023
On 11/07/23
On 13/07/23
On 14/07/23
PAST HISTORY-
K/c/o DM since 15 years on OHA
Shifted to insulin 1 year back
K/c/o CKD since 4 month and on conservative management
On regular checkup checkup was diagnosed as having HTN since 2 years and is on regular medication.
FAMILY HISTORY-
No significant family history
PERSONAL HISTORY-
Diet - mixed
Previously he used to have,gatka in morning and rice in afternoon and night ,but since 4 months gatka in the morning ,rice afternoon ,java at 3pm and at 8pm.
Appetite - decreased since 10 days
Bowel and bladder- constipation since 15 days
Addictions- chronic alcoholic since 30 years , stopped 3 years ago , smoker for 20 years stopped 2 years ago
GENERAL EXAMINATION-
Patient is conscious, coherent and cooperative
Orientation
Moderately built and nourished
Pallor- absent
Icterus-absent
Cyanosis-absent
Lymphadenopathy-absent
Edema-absent
At the Time of admission
VITALS
BP- 150/70 mmHg
PR-98 bpm
GCS- E4V1M6
RR- 18cpm
SYSTEMIC EXAMINATION-
Respiratory system-
INSPECTION-
Shape - round large with no distension
Umbilicus - inverted
Equal symmetrical movements in all quadrants with respiration
No visible pulsations , palpations , dilated veins or localised swelling
PALPITATION -
No local rise of temperature
No tenderness
No organometaly
PERCUSSION- liver dullness heard at 5th intercostal space
AUSCULTATION-
Bowel sounds present
No bruit heard
Right Left
Spinothalmic
1. Crude touch- + +
2. Pain- + +
3.Temperature- + +
Posterior Coloumn
1. Fine touch + +
2.Vibration Felt Felt
( over bony prominence )
MOTOR EXAMINATION
Tone
UL- Increased N
LL- Increased N
Power
UL- 4/5 4/5
LL- 4/5 4/5
Reflexs
B +3 +3
T +2 +2
S - -
K +2 +2
A - -
Plantars Flexor Flexor








































Comments
Post a Comment