March 16 ,2023
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
Blog by Janhavi Virani
A 35 year old female resident of Nakrikal who is a daily wage labourer by occupation came with
CHIEF COMPLAINTS of :-
1. Fever since 1 week
2. Headache since 1 week
HOPI :-
Patient was apparently asymptomatic 1 week back then she developed fever which is intermittent in onset ( on and off ) increasing at night time and decreasing in the morning associated with chills and headache ( increased headache leading to increase in fever ).
Fever is relieved by taking anti pyretic . No history of nausea , vomiting , rash or body pain .
History of unilateral headache since 1 week which is severe throbbing pain in left fronto parietal occipital region radiating to the neck due to exposure of stress . Pain is causing her to wake up at night ( inadequate sleep ) .
Headache is associated with vomiting ( just 1 episode ) phonophobia and blurring of vision ( history of change in spectacles) , decreased regular physical activity , tingling sensation in hand and feet . It relieves on taking rest and medication .
No history of aura , photophobia , depression , irritability, cravings , diarrhoea/constipation.
She has history of burning micturition since 5 days associated with decreased urine output, decreased frequency, left loin pain which is dragging type pain ( since 1 day ) . No aggrevating and relieving factors . No history of urgency, hematuria , nausea , vomiting .
DAILY ROUTINE:-
She gets up at at around 5 in the morning does her daily chores and gets her kids ready for school then she has breakfast at 8:30 or 9 am and then sleeps for sometime before she goes to work which she has stopped going since 6 years .
PAST HISTORY:-
Similar episode one year back .
Not a known case of Diabetes, hypertension, epilepsy, cardiovascular disease and tuberculosis.
History of hypothyroidism 10 years back for which she is on daily thyroxine ( 75 mg ) supplements.
History of renal stones in the left kidney 6 years back for which she took conservative treatment.
FAMILY HISTORY :-
No significant family history .
PERSONAL HISTORY:-
Diet - mixed
Appetite - decreased
Sleep- inadequate
B&B - she is constipated
Addictions- none
NO H/o is any drug allergy
GENERAL EXAMINATION:-
Patient is conscious, coherent and cooperative
Well oriented to time. Place and person .
Moderately built and nourished
O/E - thyroid appears normal
Clubbed- absent
Cyanosis- absent
Icterus - absent
Generalised lymphadenopathy- absent Edema - absent
FEVER CHART :-
VITALS:-
Temp - 99 F
PR - 84bpm
RR- 20 cpm
BP - 100/70 mm of Hg
SYSTEMIC EXAMINATION:-
CVS - S1 S2 heard , no murmurs present
RESP - bilateral Air entry present
normal vesicular breath sounds heard
ABDOMINAL-
examination of oral cavity is normal
**Inspection
-shape-normal(rounded)
-no flank fullness is seen.
-skin-no scars seen ,presence of striae.
-no dilated veins seen
-Movements of abdominal wall-no visible peristalsis,no visible pulsations
-umbilicus-inverted.
**Palpation
-tenderness-hypogastrium and left lumbar region
-warmth- present (fever)
-rigidity,guarding is absent
*no organomegaly, normal bowel sounds heard
CNS:no focal deficits are found.
Higher mental functions- normal
Brudzinski’s sign - absent
Kernig’s sign - absent
PROVISIONAL DIAGNOSIS:-
Migraine/ Left Renal Calculi / UTI
INVESTIGATIONS:-
Complete urine examination:-
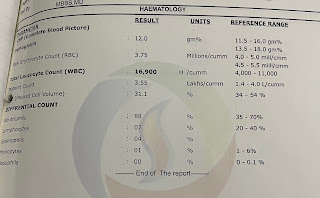
Hemogram :-
Thyroid profiles :-
USG :-
TREATMENT:-
Inj-optineuron 1amp in 100ml of NS OD
IvF-@70ml/hr
Tab nitrofurantoin 100mg
Tab pan
Tab naproxen 250mg
Bp,temp,RR,PR check 4th hrly
Tab thyronorm 25mcg







Comments
Post a Comment