This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS :
A 50 year old male patient who is painter by occupation and resident Mamidala was brought to casualty with complaints of
1. SOB since 1 day
2. Fever since 3 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 months back then he developed sudden onset SOB , chest pain , palpitations at midnight and was taken to hospital. He was found to have high BP ( SBP of 220mmHg ) and was managed conservatively.
Since then patient is having episodes of fever and SOB .
Fever is associated with chills and rigor which relieved on taking medication No history of vomiting , loose stools
SOB with exertion ,
Paroxysmal Nocturnal Dyspnea present which relieved on taking nebulisation Not associated with cough .
Patient has gotten dialysis done 5 times since 31/5/23
PAST HISTORY:
No similar complaints in the past
He is a K/C/O HTN since 3 months and taking following medication (Tab Nicardia 20mg TID , Tab Arkamin 0.1 TID , Tab Met-XL 25mg OD )
K/C/O CAD ( Stable Angina )
K/C/O CKD since 2 months
Not a K/C/O DM , TB , Asthma , Epilepsy
PERSONAL HISTORY:
Diet - mixed
Appetites - normal
Sleep - adequate
Bowel and bladder - regular
H/o burning micturition since 2 months
Decreased in urinary frequency since / months
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
Patient is drowsy , Arousable
Patient is moderately built and nourished
BP - 100/70 mmHg
PR - 109 bpm
RR - 48
Temp - 99F
Spo2- 98% on 4l of o2
No pallor , icterus , cyanosis , generalised lymphadenopathy , clubbing , pedal Edema
SYSTEMIC EXAMINATION:
CVS :
Inspection - percordium is normal
Position of trachea is central
No visible scars , sinuses , pulsations
No dilated or engorged veins
Palpation -no local rise of temperature , no tenderness
position of trachea is central
Apex beat in 6th intercostal space away from midclavicular line
No palpable thrills or heave
JVP not raised
Auscultation- S1 S2 heard , no murmurs
RESPIRATORY SYSTEM:
Inspection:-
oral cavity- Normal ,nose- normal ,pharynx-normal
Shape of chest - normal
Chest movements : bilaterally symmetrically
Trachea is central in position.
Palpation:-
All inspiratory findings are confirmed
Chest movements bilaterally symmetrical
AUSCULTATION
BAE+, NVBS
PER ABDOMINAL:
Soft , non tender
No organomegally
Bowel sounds heard
CNS :
No focal neurological deficit’s present
INVESTIGATIONS :
Chest X- Ray
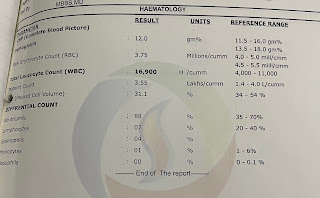
LABS:
DIAGNOSIS:
CKD ON MHD
HFpEF (EF = 54%) secondary to CAD ( stable angina )
TREATMENT:
Fluid restriction < 2L / day
Salt restriction
Inj Peptaz 2.25g iv/tid
Inj Lasix 40mg iv/BD
T. Clopitab 150 mg RT/od
T. Atorvas 40mg RT/HS
T. Nicardia 20mg RT/ Tid
T. Arkamin 0.1mg RT/ Tid
T. Met-xl 50mg RT/od
T. Nodosis
T. Shelcal
Inj. Erythropoietin
T. Orofer















Comments
Post a Comment